Advancing Treatment,
Advancing Lives.
Highest level of ethical standards &
professional excellence in oncological care.
professional excellence in oncological care.



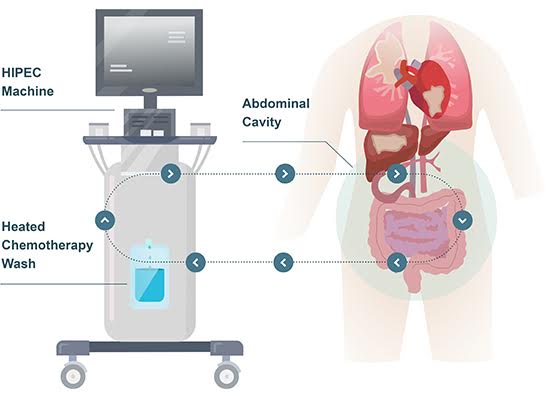
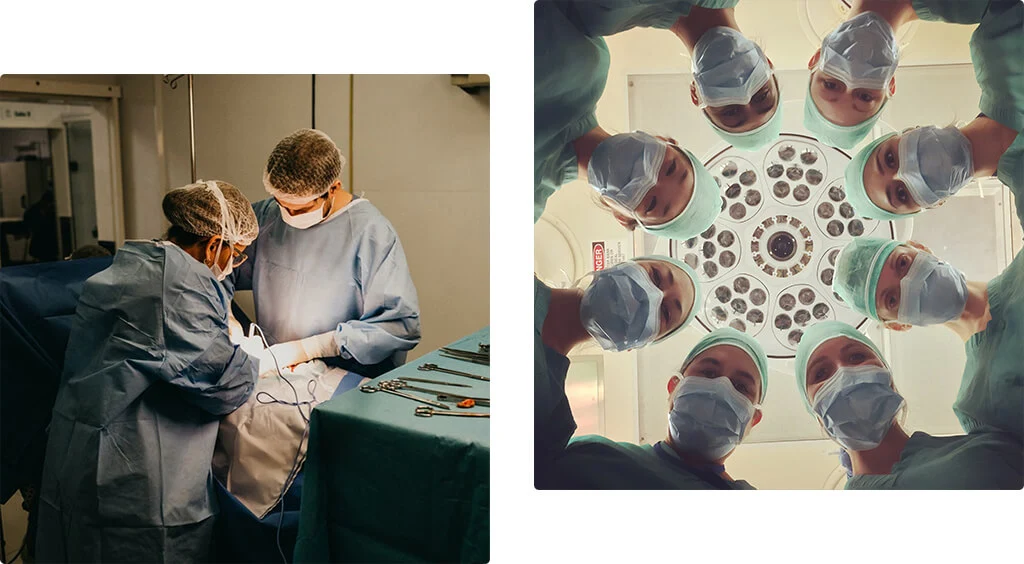
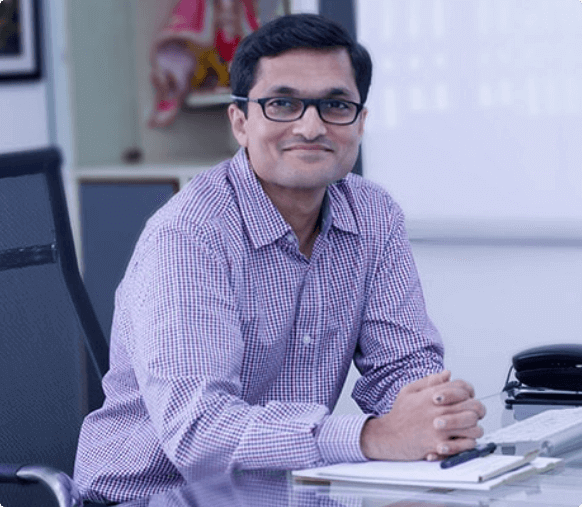
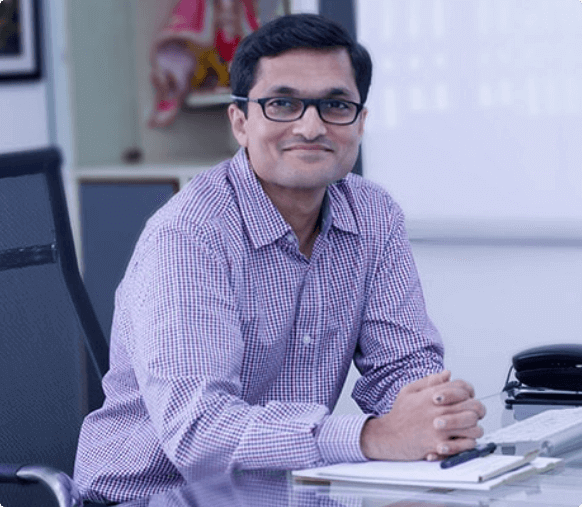
Leading the vanguard of Cytoreductive Surgery (CRS) and HIPEC in the country, Dr. Sanket Mehta focuses on the quality of care with surgical proficiency and patient centric treatment. The highest quality services are an amalgamation of complex procedures, medical expertise, a humane touch and a vision of excellence.
A Vision
of Excellence
Leading the vanguard of Cytoreductive Surgery (CRS) and HIPEC in the country, Dr. Sanket Mehta focuses on the quality of care with surgical proficiency and patient centric treatment. The highest quality services are an amalgamation of complex procedures, medical expertise, a humane touch and a vision of excellence.
Pioneer of
CRS & HIPEC


Surgeries
1000+


Years of experience
11+
Modern Oncological Treatment of International Standards





Highest Standards of Patient Care & Safety
Highest Standards of Patient Care & Safety
With 11+ years of medical experience Dr. Mehta offers world-class diagnostic, therapeutic and
rehabilitative care of the highest standards.
Hear It From
Our Patients
[sp_testimonial id="268" ]
Medreads







Gastrointestinal & Colon Cancers
2 September, 2021


Peritoneal Mesothelioma
1 September, 2021


Ovarian Cancer
31 August, 2021


Rectum Cancer
30 August, 2021





Our Publications
3 July, 2021
Human papillomavirus infection: Is it associated with epithelial ovarian cancer?
VIEW FULL ARTICLE
21 January, 2021
Pattern of recurrence after interval cytoreductive surgery and HIPEC following neoadjuvant chemotherapy in primary advanced stage IIIC/IVA epithelial ovarian cancer
VIEW FULL ARTICLE
1 January, 2021
Distribution of residual disease in the peritoneum following neoadjuvant chemotherapy in advanced epithelial ovarian cancer and its potential therapeutic implications
VIEW FULL ARTICLE
18 November, 2020
Clinical and Radiologic Predictors of a Pathologic Complete Response to Neoadjuvant Chemotherapy (NACT) in Patients Undergoing Cytoreductive Surgery for Colorectal Peritoneal Metastases: Results of a Prospective Multi-center Study
VIEW FULL ARTICLE
29 August, 2020
Current practice of pressurized intraperitoneal aerosol chemotherapy (PIPAC): Still standardized or on the verge of diversification?
VIEW FULL ARTICLE